Dysphagia is a swallowing disorder that affects the way a person eats and drinks. It must be treated quickly in order to ensure the person can eat safely and get adequate nutrition.
Dysphagia is treated with swallowing therapy. This therapy is provided by speech therapists who specialize in feeding and swallowing therapy. Keep reading to learn more about the causes and symptoms of swallowing disorders and how dysphagia is treated.
What is dysphagia?
Dysphagia is a swallowing disorder. There are four main types of swallowing problems in adults:
1 Oral dysphagia
Involves swallowing difficulties in the oral cavity, such as the lips, tongue, and soft palate
2 Pharyngeal dysphagia
Involves swallowing problems in the throat
3 Esophageal dysphagia
Involves swallowing difficulty in the esophagus
4 Gastroesophageal junction dysphagia
Involves swallowing problems at the connection point between the esophagus and the stomach
These dysphagia types can also occur together, meaning a person can have oral and pharyngeal dysphagia at the same time (known as oropharyngeal dysphagia).
Find the right speech therapist for you
We'll match you with a speech therapist who's experienced in your area of need and available when you are.
 Get started
Get startedHow common is dysphagia?
According to the American Speech-Language-Hearing Association (ASHA), it’s estimated that 1 in 25 adults experiences a swallowing problem each year. Because dysphagia occurs across many age groups and co-occurs with many diseases, the prevalence is not fully known. However, we do know that swallowing issues are more common among older adults and are associated with age-related muscle weakness (known as sarcopenia) or changes in bone structure within the neck or upper back.
What causes swallowing problems?
What diseases can affect swallowing? Dysphagia can be related to nerve and/or brain damage associated with stroke, traumatic brain injury (TBI), spinal cord injury, head and neck cancer, multiple sclerosis (MS), Lou Gehrig's disease (ALS), dementia, Parkinson’s disease, and other neurological diseases.
Swallowing problems can also be associated with pulmonary diseases, acid reflux, muscle weakness, and side effects from certain medications.

Signs and symptoms of swallowing disorders
Signs and symptoms of swallowing problems are different for each person. They can vary depending on the type of dysphagia. Some of the signs and symptoms of dysphagia include:
Drooling and/or difficulty managing food and liquids
Extra time and effort needed to chew and swallow
Unexplained weight loss
Pain when swallowing
Feeling like food is stuck in the throat (known as globus sensation)
Wet or gurgly voice during or after eating and drinking
Coughing/choking during or after eating and drinking
Difficulty coordinating breathing and swallowing
Recurrent pneumonia (due to aspirating food or liquid, which is when food or liquid enters the airway)
Who treats dysphagia?
Speech-language pathologists, also known as speech therapists, play an essential role in assessing, treating, and managing swallowing disorders. They work along with other healthcare providers, like head and neck surgeons (ENTs), gastroenterologists (GI doctors), and even physical therapists, to assist with proper positioning when eating.
Speech therapists are trained to recognize signs of esophageal and gastroesophageal dysphagia. They can then refer the person to the right health care professional. Patients with progressive diseases and those within end-of-life care can also benefit from treatment with a speech therapist.

When should you be worried about trouble swallowing?
It's important to know that dysphagia can cause medical complications, including aspiration pneumonia, malnutrition, and dehydration.
Aspiration pneumonia: Swallowing difficulties can impact the body’s ability to protect the person’s airway, allowing food, liquid, and/or bacteria to reach the lungs. This is known as aspiration. Aspiration happens most often when a person becomes weak or injured and is no longer able to feed themselves and requires assistance with eating. Recurring episodes of aspiration can lead to upper respiratory infections and pneumonia. And sadly, pneumonia is the leading cause of death within older adults.
Malnutrition/dehydration: Malnutrition and/or dehydration can also occur if a person is not able to eat or drink enough because of their swallowing difficulties. When people have discomfort with swallowing, they may eat less than is needed for their caloric intake.
Dysphagia can impact many areas of a person’s life. In addition to medical complications, a person with dysphagia may have less interest or enjoyment related to eating and drinking. They may feel embarrassed and avoid social gatherings. In some cases, they may need diet modifications that significantly limit what they can eat.
Caregivers and family members of those with dysphagia can also feel a burden to ensure the safety of their loved one.


What happens during an evaluation for dysphagia
If you or a loved one is having trouble swallowing, speak with your doctor. They can refer you to a speech-language pathologist for an evaluation. Speech therapists are the most qualified providers of dysphagia services because of their unique training.
The speech therapist will perform tests to gain a better understanding of your diagnosis and create a personalized treatment plan. The evaluation may include:
Screening – Pass/fail to determine if further testing is needed.
Review of your medical history – To learn more about your concerns, medical conditions, and any other contributing factors.
Oral mechanism and/or cranial nerve examinations – To assess the structures and muscles involved in swallowing, your ability to cough and throat clear, your head/neck control, etc.
Clinical swallow assessment – Trying food and liquids of varying consistencies and thickness while assessing your oral control and watching for signs or symptoms of aspiration.
Diagnostic tests with imaging – Allows speech therapists to evaluate the anatomy and physiology of the structures used for swallowing in order to determine if dysphagia is present and its severity, possible causes, and other clinical factors. Two diagnostic imaging tests can be done:
Videofluoroscopic Swallowing Study (VFSS) – Video swallow studies use barium and a moving X-ray. They are performed in the radiology suite.
Flexible Endoscopic Evaluation of Swallowing (FEES) – FEES uses a nasal endoscope. It can be performed in an outpatient setting or at the person’s bedside in many different medical environments.


Treatment for swallowing problems
How do you fix difficulty swallowing? Treatment for swallowing difficulty is individualized. Treatment varies for each person based on the cause(s), symptom(s), and type of dysphagia. Speech therapists create a treatment plan that will improve a person’s swallow safety, support their nutrition and hydration, and improve their quality of life.
You can learn more about Expressable's dysphagia program in our treatment guide. Treatment for swallowing problems can include the following elements:
Exercises
Exercises are used to rehabilitate your swallowing skills by improving your physiological functions, such as strength, range of motion, and coordination. There are a variety of exercises that will be chosen by your speech therapist to fit your individual needs.
Compensatory strategies
These strategies are used to improve the safety and effectiveness of your swallow. They involve changes to how you consume food and liquids. Compensatory strategies might include pacing how you eat and drink, as well as changing your posture. It’s important to note that compensatory strategies do not improve your function over time like exercises do.
Changes to diet
Diet changes are made to help you swallow safely. Your speech therapist might recommend changing the texture and/or thickness of your food and liquid in order to improve feeding safety. You might also change how your food is prepared, such as by chopping or pureeing it. The taste and/or temperature of the food can be changed to increase your enjoyment of it as well.
Other techniques
Other tools and exercises to treat dysphagia include swallow maneuvers, oral care education*, adaptive equipment, environmental modifications, sensory stimulation techniques, prosthetics, and feeding tubes. For people who need assistance with eating, an important goal will be to work toward regaining their ability to feed themselves in order to reduce the risk of aspiration.
*A clean mouth greatly improves the safety of a swallow. Aspiration of bacteria in the mouth creates a significant health risk.

How is treatment for dysphagia delivered?
According to ASHA, individuals diagnosed with dysphagia can receive therapy in various ways. Dysphagia therapy can be one-on-one, as part of a group during mealtime, and via telepractice, or online therapy.
What does teletherapy for dysphagia look like?
Some types of swallowing therapy can be done through teletherapy, but not all. Some people may need the therapist to be physically present for safety reasons. This decision should be made by the patient's doctor and a speech therapist who specializes in swallowing. The speech therapist will consider the person’s diagnosis, severity of swallowing problems, current condition, and goals.
The therapist will teach the patient and their caregiver about signs of aspiration, compensatory swallowing strategies, and any necessary changes to the person’s diet.
Dysphagia teletherapy requires planning and communication among the speech therapist, patient, and/or their caregiver. Certain foods and liquids may need to be used during sessions as exercises and strategies are practiced. A caregiver or support person must be present during sessions for safety and support. They can help prepare any foods and liquids and help ensure the person is positioned and equipped correctly.
In swallowing therapy, the therapist will teach the patient and their caregiver about signs of aspiration, compensatory swallowing strategies, and any necessary changes to the person’s diet. The caregiver plays a key role in learning swallowing exercises alongside the patient to help them practice at home between sessions. Overall, teletherapy for dysphagia relies on teamwork!
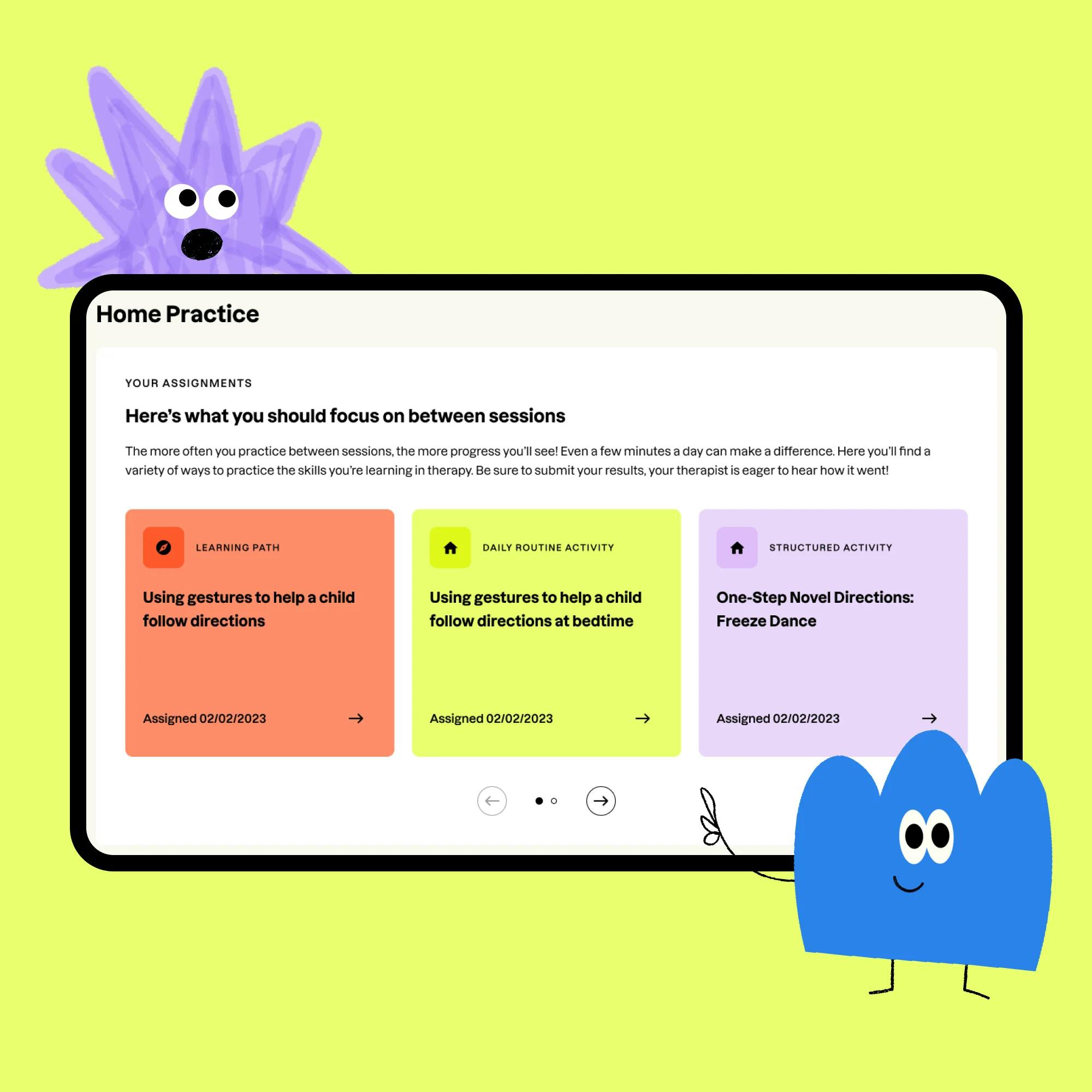
Support beyond sessions: The Expressable portal
Your swallowing therapy doesn’t stop when the session ends. At Expressable, you and your loved ones will get access to our client portal, which makes practicing swallowing strategies easier and more effective. Here’s what you’ll find:
Learning Paths that explain and reinforce feeding therapy strategies
Demo videos that show real swallowing techniques in action
Home practice activities you can do during your everyday meals and routines
Text messaging support so you can ask questions, get reminders, or receive tips from your therapist between sessions.
By using the tools in the portal and practicing regularly, you can make faster progress and build more independence in your feeding abilities.

What to do next if you have concerns about swallowing
If you think you might have a swallowing problem, talk with your doctor to rule out or discover any underlying condition(s). It’s also important to seek a referral for an evaluation by a speech-language pathologist. Speech therapists are an essential part of the health care team for dysphagia management. Click here to get matched with an Expressable speech therapist who specializes in swallowing therapy.
When talking with your doctor, be prepared to discuss times of day or anything you do that makes the problem better or worse. You should also discuss medications, medical conditions, and any other concerns or symptoms you’re experiencing.
Additional resources
For more information about swallowing disorders, please visit these organizations: ASHA, The National Foundation of Swallowing Disorders, and the Mayo Clinic.
How Expressable Can Help
Concerned your child isn't reaching age-expected milestones? Looking for communication support from a professional? Expressable is a national online speech therapy practice serving children and adults. We treat all major areas of communication and feeding, offer flexible hours including evenings and weekends, and accept most major health insurance plans. We’re proud to have earned more than 3,000 5-star reviews from our clients (4.9/5 average).
Our therapy model is centered on parent and caregiver involvement. Research proves that empowering caregivers to participate in their loved one’s therapy leads to better outcomes. That’s why we combine live, 1-on-1 speech therapy with personalized education and home practice activities for faster progress.
Communication is more than words. It’s how we share how we feel and show who we are. We’re here to help you or your child do just that.

 Alexis Irazoque, M.S., CCC-SLP
Alexis Irazoque, M.S., CCC-SLP